Presentation- Dual Diagnosis Trends: Implications and Treatment Recommendations for Teens and Young Adults
This presentation provides an overview of the relationship between adolescent and young adult mental health and substance use disorders, and its implications for patients, practitioners, and services. Participants will increase their understanding of dual diagnosis, types of treatment and levels of care, and components of treatment that impact positive treatment outcomes.
Learning Objectives
State 3 links between substance use and mental health disorders in adolescents and young adults.
Identify 3 risk and protective factors of substance use disorder.
Identify at least one component of adolescent and young adult treatment that increases positive outcomes.
Check out the full presentation or read below.
Overview
What is Dual Diagnosis? Dual Diagnosis is having both a mental health disorder and substance use disorder simultaneously. The term co-occurring is also commonly used to describe having both disorders.
According to the 2020 National survey on Drug use and Health, 73.8 Million American adults had a substance use disorder or some kind of mental illness and 17 million had a dual diagnosis. Of those 73.8 million only 48% received some kind of treatment and only 6% of the people with a dual diagnosis received treatment that addressed both substance use AND mental health. If people with a dual diagnosis did receive treatment it was most common for them to receive MH treatment only as you can see with 42.3%
Research also shows that the number of teens and young adults with a dual diagnosis is rising and that they’re less likely to receive treatment for their SUD than adults. It was also noted that the percentage of people aged 12 or older with an alcohol use disorder was highest among young adults aged 18-25 (5.2 million people).
Marijuana use was also highest among young adults. Adolescents who had a major depressive episode and young adults with any mental illness were found to be more likely to have used substances over the past year so its really important to assess for and address substance use in Mental health settings and vice versa.
Link Between Mental Health & Substance Use:
The relationship between SUDs and mental disorders is known to be bidirectional. So basically, mental health can impact substance use disorders and substance use disorders can impact mental health. The combined presence of SUDs and MH disorders results in:
· More profound functional impairment
· Worse treatment outcomes
· Higher morbidity and mortality
· Increased treatment costs
· Higher risk for homelessness, incarceration, and suicide
Current treatment guidelines recommend that people with co-occurring disorders receive treatment for both disorders. Unfortunately, as the stats show, many people don’t receive treatment for either and if they do, its often not for both.
Its important to note that 30-45% of adolescents and young adults with Mental health disorders have a co-occurring substance use disorder.
At Serenity, we often see high schoolers who enter treatment due to anxiety, depression, and marijuana use and work towards increasing their awareness on how MH and SU impact one another.
We’ve also have noticed that a lot of teens come in believing that marijuana is not harmful for them and helps their anxiety, when in reality, studies show that teen marijuana use is linked to increased depression and suicidal ideation. Research also shows decrease in IQ.
Despite the negative outcomes, many teens do not receive substance use treatment. Even though there has been an overall decrease in stigmas surrounding substance use, it still seems to be a barrier for seeking treatment.
At times parents may express concern about their teen (or young adult) participating in treatment with others who are also using substances and fear their child will be negatively influenced. Clients and Parents also report concern regarding the impact a substance use diagnosis may have on their child’s future.
To combat this barrier to treatment we often provide psychoeducation and highlight the benefits of receiving both mental health and substance use treatment as well as benefits of group therapy and peer support. Check out this blog post for more information on the benefits of group therapy.
Mental Health and Substance Use Warning Signs
Some of the most common warning signs we see at Serenity are changes in friend group, increased family conflict, lack of motivation, feelings of loneliness and hopelessness and not knowing how to express themselves or attempting to cope by isolating. It’s important to look out for some of these warning signs and to remember that changes can happen slowly over time and the abnormal can begin to seem normal.
What Works for Teens & Young Adults
So, what works for teens & young adults? Treating substance use disorders and mental health disorders concurrently requires a comprehensive and well rounded treatment plan that incorporates a variety of services that address both disorders. Often times this includes CBT, Motivational interviewing, contingency management, family involvement, 12 step/support meetings, medication management, group therapy and the others listed have all been shown to have a positive impact on treatment outcomes. Two that really stand out to us at Serenity are group and family therapy.
Working with teens & young adults we’ve seen how effective group and family therapy can be. Studies show that people who engage in group therapy communicate more spontaneously and freely, build community connections, and have better treatment outcomes. It gives them the opportunity to provide and receive feedback, develop social skills, and have a sense of community and trust. Plus, sometimes receiving feedback from a peer can be way more effective than hearing it from a parent or therapist. Our teens will be the first to tell us that.
Often times, young adults will come to us for treatment while struggling in college or taking a leave from college and things like collegiate recovery, sober dorms, and 12 step meetings while attending treatment can be very helpful. It’s also important to set up aftercare so clients leave treatment with the appropriate resources like sober living, support groups, or ongoing treatment etc.
Lets talk a little more about groups… At Serenity we like to meet the clients where they are and allow flexibility within our groups. We incorporate psychoeducation on specific themes and topics that we see emerging in groups. Some days we can tell that group members would rather a process group so we will allow them to work through whatever is coming up for them at that time.
We also create and incorporate activities to keep things fun, educational, and therapeutic. Obviously, therapy is hard work but it can also be fun and engaging for young people. A lot of times, the kids will come to us and share how much they liked being able to connect with their peers and receive support. One of the most common things I hear is how relieved they were to learn they weren’t alone and that other people their age are experiencing similar things.
Another common topic that comes up in group is family conflict and/or how to improve relationships with family members. This also shows the importance of incorporating family therapy into treatment.
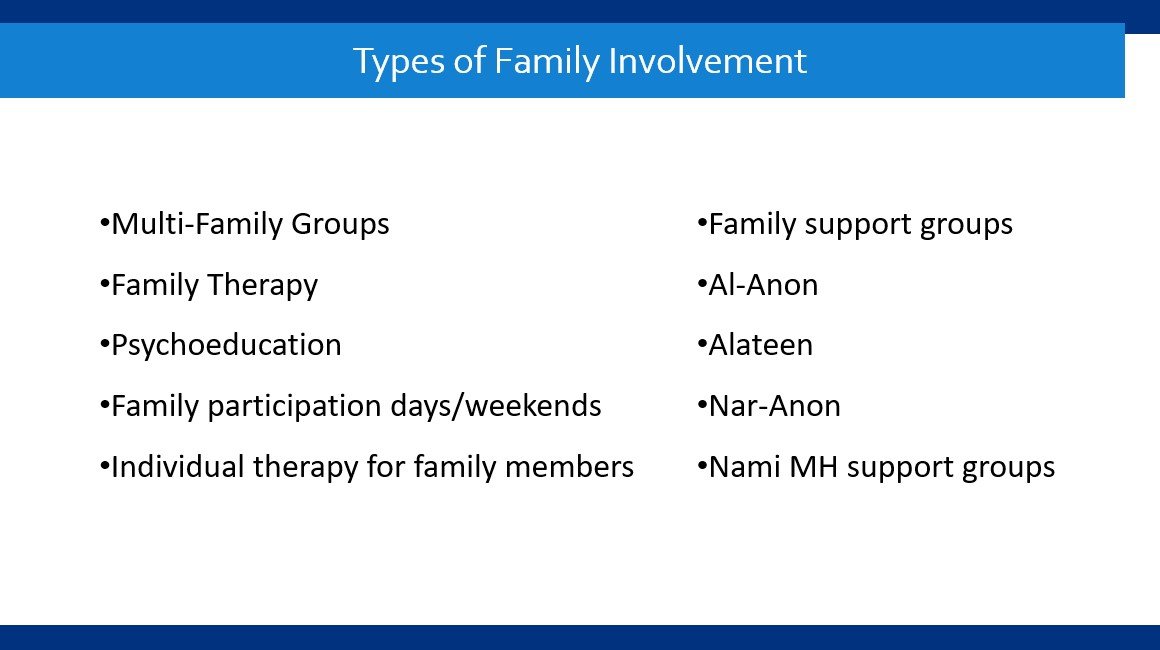
Family dynamics can have a large impact on substance use and vice versa, especially when working with teens and young adults. High levels of relationship dysfunction and conflict, and low family support may contribute to substance use, while substance use of a family member can also contribute to such family dysfunction. We can do great work with the individual, but it can be really difficult for long lasting change to occur if we’re not also working with the family they’re going home to every day. There are many different types of family involvement that programs offer and that can be helpful for teens and young adults.
Types of Family Involvement
Family involvement can be an incredible tool to clients. Family involvement however, is more than just family therapy and there are many different ways family members can get involved while also utilizing their own support.
Through family involvement, caregivers can learn to recognize behaviors consistent with SUDs as symptoms rather than simply, choices (e.g., lying/deception, denial, and relapse). Therapists can assist caregivers in identifying family interactions that may cue or trigger distress in the SUD family member and learn to approach those interactions differently.
Family members themselves may have developed their own maladaptive, symptomatic, often fear-based behavior in relationship to their SUD loved one and could benefit from support for themselves. Often times a referral for a parent or family member to seek their own counseling may be beneficial.
At Serenity we offer a parent support group and family therapy but also encourage involvement in additional support groups like Al-anon, Naranon and Nami mental health support groups. For those of you who may not be familiar with some of these support groups, Al-anon, Nar-Anon, and Alateen are support groups for people who have loved ones struggling with addiction.
Al-anon is specifically for alcohol, Nar-Anon is specifically for substances and Alateen and Narateen are the groups specifically for teens who have a loved one struggling with addiction. I’ve noticed that client’s whose parents and families engage in some form of family involvement often feel more supported, understood and seem to have better treatment outcomes. Check out our resources page for local information about these groups.
Impact of Family Therapy
Some of the benefits of family therapy are increasing family cohesion, improving overall family functioning, and adopting new solutions within the family. Early intervention and family involvement in adolescence can reduce risk for the future. Within family therapy, family members can increase their understanding of the "problem" and the impact that the family dynamic may have. Parents often learn healthier parenting practices and generally report higher satisfaction as a parent after doing so.
Generally, members in family therapy feel safe due to having a mediator. Therapists can address the elephants in the room or certain behavioral patterns that may have been the norm within the family. The intensity and type of family involvement varies among treatment providers and levels of care so its important to have an understanding of your clients needs.
Levels of care
Level of care generally refers to the intensity of services that are required to diagnose and treat a condition. Clients can move through different levels of care as their treatment needs change. A higher level of care like IOP, that incorporates services in addition to individual therapy can be very helpful and at times necessary when working with clients with a dual diagnosis.
References
Baker, A. L., Thornton, L. K., Hiles, S., Hides, L., & Lubman, D. I. (2012). Psychological interventions for alcohol misuse among people with co-occurring depression or anxiety disorders: A systematic review. Journal of Affective Disorders, 139(3),
217–229. https://doi.org/10.1016/j.jad.2011.08.004Blanco, C., Alegria, A. A., Liu, S. M., Secades-Villa, R., Sugaya, L., Davies, C., & Nunes, E. V. (2012). Differences among major depressive disorder with and without co-occurring substance use disorders and substance-induced depressive
disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry, 73(6), 865–873. doi:10.4088/JCP.10m06673Substance Abuse and Mental Health Services Administration. (2020). Substance Use Disorder Treatment for People with Co-Occurring Disorders. Treatment Improvement Protocol (TIP) Series 42 Publication No. PEP20-02-01-004. Rockville, MD: Substance Abuse and Mental Health Services Administration
Hogue, A., Henderson, C. E., Becker, S. J., & Knight, D. K. (2018). Evidence base on outpatient behavioral treatments for adolescent substance use, 2014–2017: Outcomes, treatment
delivery, and Promising Horizons. Journal of Clinical Child & Adolescent Psychology, 47(4), 499–526. https://doi.org/10.1080/15374416.2018.1466307Jiménez, L., Hidalgo, V., Baena, S., León, A., & Lorence, B. (2019). Effectiveness of Structural⁻Strategic
Family Therapy in the Treatment of Adolescents with Mental Health Problems and Their
Families. International journal of environmental research and public health, 16(7), 1255. https://doi.org/10.3390/ijerph16071255
Nawi, A. M., Ismail, R., Ibrahim, F., Hassan, M. R., Manaf, M., Amit, N., Ibrahim, N., & Shafurdin, N. S.
(2021). Risk and protective factors of drug abuse among adolescents: a systematic review. BMC public health, 21(1), 2088. https://doi.org/10.1186/s12889-021-11906-2
Nelson, S., Van Ryzin, M., & Dishion, T. (2015). Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: Demographic correlates and young adult substance use problems. Development and Psychopathology, 27(1), 253-277.
doi:10.1017/S0954579414000650Tambling, R. R., Russell, B., & D, A. C. (2021). Where is the Family in Young Adult Substance Use Treatment? The Case for Systemic Family Therapy for Young Adults with Substance Use Disorders. International Journal of Mental Health &
Addiction, 1–12. https://doi-org.dbproxy.lasalle.edu/10.1007/s11469-020-00471-1Sarvey, D., & Welsh, J. W. (2021). Adolescent substance use: Challenges and opportunities related to COVID-19. Journal of Substance Abuse Treatment, 122, 108212. https://doi.org/10.1016/j.jsat.2020.108212
Substance Abuse and Mental Health Services Administration. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-
003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/Squeglia Lindsay, M., Fadus, M. C., McClure, E. A., Tomko, R. L., & Gray, K. M. (2019). Pharmacological treatment of youth substance use disorders. Journal of Child and Adolescent Psychopharmacology, 29(7), 559-572.
doi: http://dx.doi.org/10.1089/cap.2019.0009Justin R. Watts, Dalia Chowdhury & Linda Holloway (2019) Success in collegiate recovery programs: results from a phenomenological investigation, Alcoholism Treatment Quarterly, 37:2, 163-180, DOI: 10.1080/07347324.2018.1532776